- Did you know? Over 50% of VA secondary claims are initially denied due to missing evidence or unclear secondary conditions. Many veterans wait months—sometimes years—for the compensation they deserve, but with the right approach, you can dramatically increase your chances for faster approval.
Understanding VA Secondary Claims: The Path to Faster Approval
- Explore what VA secondary claims are, why they matter to your disability compensation, and set out practical steps to accelerate your approval process.
- Real-life scenarios show how establishing a secondary condition can impact your total disability rating and monthly compensation.
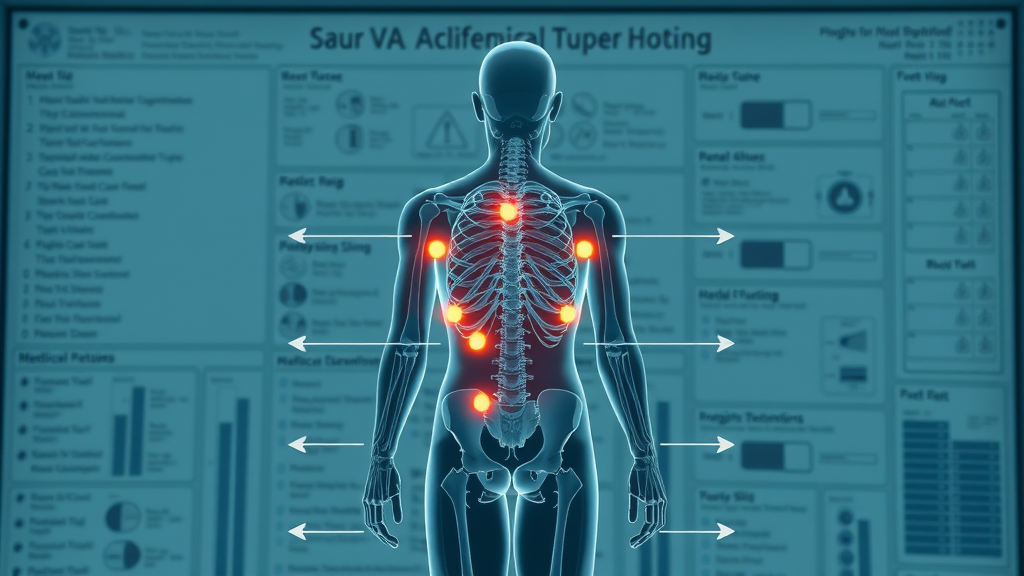
Navigating the VA disability system is challenging—even more so when you're dealing with secondary conditions that stem from your primary, service-connected disabilities. Many veterans aren't aware that these secondary service issues, like depression due to chronic pain or migraines stemming from traumatic brain injury, can (and should) be claimed for additional compensation. The VA acknowledges that certain new disabilities can result either directly or indirectly from conditions for which you already receive benefits.
When filing VA secondary claims , understanding the regulations and documenting each condition properly can make a dramatic difference in outcomes. For example, a veteran with a primary disability rating for a knee injury who later develops hip problems—or chronic headaches because of post-traumatic stress disorder—may qualify for a higher combined rating and additional monthly disability compensation. Real-world cases demonstrate that thoroughly linking your disability claim to secondary conditions, and submitting clear, credible medical evidence, speeds up the VA's approval process and can significantly boost your total support.
Essential Elements of a Successful VA Secondary Claim
Defining Secondary Conditions Under VA Regulations
- How does the VA differentiate primary and secondary conditions?
- Recognizing common secondary conditions linked to established disabilities.
The VA differentiates primary conditions from secondary conditions based on direct service connection. Primary (or service-connected) disabilities result from events or exposures during military service and are the foundation for your initial disability claim. A secondary condition is any new medical problem caused or aggravated by one of these service-connected disabilities. For instance, if an ankle injury worsens due to compensatory changes from a prior knee injury, the resulting ankle issue is eligible for a secondary service connection.
Veterans frequently encounter secondary conditions such as hypertension (secondary to PTSD), sleep apnea (secondary to anxiety), or chronic pain syndromes that evolve due to earlier injuries. Recognizing these options—and how they relate to your existing disability rating—will empower you to pursue all the benefits you are owed. Many successful VA secondary claims include documentation showing the medical correlation between your documented primary disability and the new secondary condition.
Connecting Your Disability Claim to Secondary Conditions
- Step-by-step process to prove your secondary claim is related to a service-connected disability.
- Sample narratives and supporting documentation.
To successfully establish a secondary service connection , you must clearly link the new medical issue to an already service-connected disability. This connection is typically demonstrated with a medical nexus letter from your treating physician, outlining how your current medical condition was directly caused or aggravated by your established disability claim. The narrative should be thorough, specific, and supported by clinical findings.
For example: “Due to the veteran’s service-connected back injury, they developed an abnormal gait, leading to hip strain, which resulted in the diagnosed arthritis in the left hip. Medical records from 2018 to present, physical therapy notes, and the orthopedic surgeon’s opinion all support this link.” Strongly worded statements backed by consistent medical evidence are your best asset when pursuing a secondary claim with the VA.
Navigating the VA Form Process for Secondary Claims
Which VA Forms Are Needed for Secondary Service Connections?
- Overview of VA Form 21-526EZ and other essential documentation.
- Tips for correctly filling out forms to avoid delays.
The VA Form 21-526EZ is the primary application for disability compensation, including for secondary conditions . Filling out this form accurately is essential. Other key documents—such as VA Form 21-4142 (Authorization to Disclose Information) and supporting service medical records—may also be required to bolster evidence to support your claim. Double-check all personal details, ensure your secondary condition descriptions match your medical evidence, and include a nexus letter whenever possible.
Avoid unnecessary delays by reviewing the instructions closely, spelling out clearly how the secondary service condition is tied to your original disability claim. Mistakes on VA forms, like missing checkboxes or omitting required supporting information, are among the most common reasons the department of veterans affairs requests additional evidence or outright denies claims.

Compiling Evidence to Support Your Secondary Condition Claim
How to Gather the Right Medical and Service Records
- Medical evidence requirements for secondary service claims.
- Getting your physician’s statement aligned with VA standards.
Medical evidence is the cornerstone of any successful secondary condition claim. This includes an up-to-date medical diagnosis, treatment records, and relevant service records substantiating your underlying primary disability. When compiling documents, clearly indicate how the secondary condition has evolved following your established service-connected condition.
To ensure your claim isn’t stalled, request that your healthcare provider draft a medical nexus statement that specifically addresses the connection between your primary disability and the secondary issue. Use straightforward language: “It is at least as likely as not that the veteran’s sleep apnea is a result of longstanding post-traumatic stress disorder related to their military service.” Aligning your medical evidence with VA requirements streamlines the process and bolsters your case for disability benefits.
Expert and Lay Evidence: Strengthening Your Disability Claim
- How buddy statements and independent medical opinions support secondary conditions.
- Sample statements that make a difference.
In addition to professional medical evidence, the VA also accepts buddy statements (firsthand observations from family, friends, or fellow service members) and independent medical opinions . These can fill in gaps, corroborate your account, and demonstrate the day-to-day impact of secondary conditions. For instance, a spouse might write, “Since his knee injury, my husband’s back pain and mobility have only worsened, making daily activities extremely difficult.”
A strong statement should provide specific examples—referencing missed work, deteriorating physical condition, or visible changes caused by the secondary service connection. Combining expert assessments, medical records, and credible lay statements will create unassailable evidence to support your claim and overcome the most common weaknesses in VA secondary claims.
Disability Compensation: Maximizing Benefits for VA Secondary Claims
How Secondary Service Connection Affects Your Overall Disability Rating
- Understanding VA math: Combining ratings for primary and secondary conditions.
- Tips to secure the highest possible monthly compensation.
Your total disability rating depends on more than the sum of individual ratings. The VA uses a complex combined ratings table, not simple addition, to determine how your disabilities interact and impact your ability to work. For example, if your primary disability is rated at 40% and your secondary at 20%, your combined rating would be 52%, which rounds down to 50%. However, stacking multiple secondary conditions can push your total disability compensation up to the next tier.
To maximize benefits, identify and document every secondary condition—no matter how minor. Request reevaluations as new symptoms develop, and always supply updated medical evidence for each disability claim. Don’t overlook the possibility of special monthly compensation if your secondary service condition triggers additional care needs or severe symptoms.

Frequently Missed Opportunities for Extra Compensation
- Special monthly compensation scenarios based on secondary service-related symptoms.
Many veterans overlook special monthly compensation (SMC) —a higher benefit available when secondary service conditions create significant obstacles, such as mobility limitations or the need for regular aid and attendance. SMC can be triggered by severe, combined disabilities such as loss of limb function, chronic pain syndromes, or mental health issues that impair daily living.
Take time to explore whether symptoms from a secondary condition —like severe depression or the need for an assistive device—warrant extra benefits. Review the official website for eligibility details, and consult a VA-accredited consultant if you’re unsure about your case.
Timeline: How Long Do VA Secondary Claims Take?
- Average processing times and factors that lead to delays for secondary claims.
- Common issues that stall decisions and how to avoid them.
The timeline for processing VA secondary claims varies, but most are reviewed within 4-8 months. However, delays can extend processing to over a year, especially if required evidence to support your claim is missing, forms are incomplete, or medical opinions are unclear. Claims are often stalled by overlooked disabilities, insufficient medical nexus statements, or missing service records.
To avoid common pitfalls, submit a complete application, follow up regularly on your claim status, and promptly respond to any VA requests for additional evidence. Being proactive and organized increases your odds of a faster, favorable decision for your disability compensation.
Secondary Claim Denials: Appeal Strategies for Veterans
Understanding Reasons for Denied Disability Claims
- The top mistakes veterans make in submitting evidence to support secondary conditions.
Disability claim denials often result from incomplete or insufficient evidence, vague medical nexus letters, missing VA forms, or failure to document progression of a secondary service connection. Veterans sometimes list only their primary condition without illustrating how additional disabilities arose as a consequence, missing a crucial step in the claims process.
Ensure every secondary condition is thoroughly explained in both medical and layperson terms. Provide recent medical records, clear timelines, and symptom progression to prevent denial and secure the disability benefits you deserve.
How to Appeal and Win a Denied Secondary Service Claim
- Supplemental vs. Higher-Level Review: Which is best for your case?
- Sample appeal letters and timelines for action.
If your VA secondary claim is denied, consider either a Supplemental Claim (submitting new and relevant evidence) or a Higher-Level Review (VA senior reviewer re-examines your file with no new evidence). The right choice depends on your situation. If you uncover new medical documentation or peer-reviewed studies tying your conditions together, a Supplemental Claim is ideal. If the denial centered on a missed administrative detail, Higher-Level Review may be faster.
When writing an appeal letter, be concise but detailed. “I am submitting new medical evidence linking my sleep apnea to my service-connected PTSD, including a nexus statement from my doctor and published literature supporting this association.” Always review the VA's official decision review process for current timelines and requirements, ensuring you don’t miss key filing deadlines.
Real Veterans, Real Results: Success Stories with Secondary Conditions
"My chronic knee pain started after years of compensating for a service-connected back injury. When I finally filed my VA secondary claim correctly, my disability compensation doubled and the process only took six months." — U.S. Army Veteran
- Additional case studies: Increased disability ratings due to PTSD secondary to traumatic brain injury, sleep apnea secondary to PTSD, and more.

Video Guide: Completing Your VA Form for Secondary Service Successfully
- A step-by-step walkthrough of VA Form 21-526EZ completion with insider tips.
Want to see the VA claim process in action? Watch our video guide for completing VA Form 21-526EZ, with real-world tips for organizing your evidence, writing effective medical narratives, and avoiding the mistakes that lead to approval delays.
Comprehensive List of Common VA Secondary Conditions
- Breakdown of the most frequently approved secondary conditions, including hypertension, depression, migraines, and more.
| Top 10 Secondary Conditions | Linked Primary Disability | Common Medical Evidence Needed |
|---|---|---|
| Hypertension | PTSD, Diabetes | Blood pressure logs, cardiology evaluations |
| Depression | Chronic pain, TBI | Psychiatric assessments, therapy notes |
| Sleep Apnea | PTSD, Anxiety | Sleep studies, mental health evaluations |
| Migraines | TBI, PTSD | Neurological exams, C&P reports |
| Radiculopathy | Back injury | Nerve conduction studies, medical imaging |
| Irritable Bowel Syndrome | Gulf War Syndrome, PTSD | GI evaluations, deployment records |
| Diabetes | Agent Orange exposure | Lab results, endocrinologist notes |
| Arthritis | Service-connected joint injuries | X-rays, orthopedic findings |
| Peripheral Neuropathy | Diabetes, spinal conditions | EMG studies, sensory exams |
| Anxiety Disorders | Chronic pain, PTSD | Psychologist statements, medical records |
Step-by-Step Checklist: Filing a Winning VA Secondary Claim
- Identify a primary, service-connected disability
- Review potential secondary conditions recognized by VA
- Consult with your treating physician for a nexus statement
- Collect all relevant medical and service records
- Complete the required VA form(s) accurately
- Attach evidence and supporting letters
- Submit your claim and track status
- Prepare for C&P exams if required

Understanding VA Disability Ratings for Secondary Conditions
The VA Rating Process for Combined Disabilities
- How secondary service influences your total disability rating.
- VA combined ratings tables explained with practical Veteran examples.
The VA uses “ VA math ” to determine combined ratings, factoring in how each additional primary or secondary condition impacts your overall level of disability. Rather than simply adding the percentages, the process involves considering the most severe disability first, then calculating subsequent conditions as percentages of your remaining “unimpaired” ability. For example, a veteran with a 40% knee injury and 20% migraine is not simply 60%; rather, it’s 40% + (20% x 60% remaining) = 52%, rounded down to 50% for compensation.
Study the VA combined ratings table and use tools at the official website of the United States department of veterans affairs to estimate possible outcomes, ensuring you don’t leave benefits on the table.
What are VA Secondary Conditions? (People Also Ask)
- Examples: Diabetes secondary to Agent Orange exposure, migraines secondary to TBI, depression secondary to chronic pain.
A VA secondary condition is any medical issue that directly results from or worsens due to a service-connected disability. Classic cases include hypertension that develops after PTSD, sleep apnea caused by service-related anxiety, or depression resulting from chronic battle injuries. These conditions are all valid for secondary service connection and may qualify you for additional monthly disability compensation.
How Far Back Does VA Pay for Secondary Claims? (People Also Ask)
- Typical effective dates for back pay and key exceptions for retroactive payments.
The VA typically pays retroactive disability compensation for secondary claims back to the date you filed your VA form or notified the department of veterans affairs about your condition. If your claim is granted, any accrued payments start from the effective date (usually the date you submitted your claim), but there can be exceptions if an earlier effective date applies—such as those involving previously denied claims that are reopened due to new and material evidence.
How Does the VA Calculate Secondary Conditions? (People Also Ask)
- Step-by-step breakdown of the VA’s combined rating system with case studies.
The VA uses a combined rating system —not simple addition—to calculate the disability rating for multiple primary and secondary conditions. For example, with a 50% service-connected PTSD and a 20% secondary sleep apnea, your total rating is 60%, not 70%. The system reduces “unimpaired” capacity as new conditions are added, so every extra secondary claim can move your rating—and monthly compensation—higher.
What Are the Top 5 Conditions Secondary to Tinnitus? (People Also Ask)
- Anxiety
- Depression
- Sleep disturbances
- Migraine headaches
- Hearing loss
- Understanding the medical literature linking these conditions to tinnitus.
Medical research confirms strong associations between tinnitus and other disabling conditions. Anxiety and depression are especially prevalent in veterans with persistent ringing in the ears. Sleep disturbances and migraines are also common, while chronic tinnitus is often linked to progressive hearing loss. Citing published literature and getting expert opinions enhances your chance of a successful secondary claim for these conditions.
Expert Tips for Gathering Evidence to Support Your VA Claim
- Insider advice on medical nexus letters, private evaluations, and avoiding common evidence pitfalls.
To maximize your chances, get a detailed nexus letter from a specialist who understands VA disability claims. Have private or independent physicians reference medical literature connecting your secondary condition to your primary disability. Always provide test results, treatment summaries, and up-to-date progress notes, and avoid relying solely on outdated or generic statements. Staying organized and submitting all evidence together prevents avoidable delays.
Video Walkthrough: Real Claims Approved—What You Can Learn
- Breakdown of successful secondary claim files, highlighting essential documentation and evidence strategies.
By reviewing real veterans’ claims that were approved, you’ll see the critical role of thorough evidence—properly filled veterans affairs forms, consistent medical histories, and strong nexus statements. Watch for strategies and best practices you can apply directly to boost your claim’s chance for prompt approval.
Answers to Frequently Asked Questions About VA Secondary Claims
- How soon after an initial approval can I file a secondary claim? You can submit a secondary claim at any time after your original service connection is established, especially if new symptoms emerge or conditions worsen.
- Can I file multiple secondary claims at the same time? Yes, you can claim as many secondary service connections as are supported by your medical and service records—just be sure each one includes specific, credible evidence.
- Does a secondary claim impact my VA healthcare eligibility? An approved secondary claim may increase your overall disability rating, potentially qualifying you for broader VA healthcare services and support.
- Guidance and best practices for each FAQ scenario.
Mistakes to Avoid When Filing for VA Secondary Service Connection
- Not providing a clear medical nexus statement
- Failing to list all possible secondary conditions
- Using insufficient or outdated medical evidence
- Missing form details or deadlines
The most common mistakes can stall or ruin your secondary claim: omitting a specific nexus letter, not listing every secondary condition that impacts your life, relying on old medical evidence, and skipping details on your VA forms. Stay vigilant, review every form, and work alongside your healthcare providers to present the strongest possible application.
Summary and Next Steps for VA Secondary Claims Success
- The critical role of complete evidence, correctly filled VA forms, and persistent follow-up.
"Preparation and perseverance are key: Veterans who present thorough medical evidence and follow up regularly see faster, more favorable results."
Ready to Secure Faster VA Secondary Claim Approval?
- Visit https://vitalveteransconsultants.com/ for one-on-one support from experienced VA claims consultants and transform your application process today.
 Add Row
Add Row  Add
Add 



 Add Row
Add Row  Add
Add 
Write A Comment